 Until my first daughter Carly was born by an ER-style emergency c-section, I had never been to the hospital except for the couple of times with minor injuries as a small child. The experience was so extraordinarily shocking to my system that it catapulted me into a determination that my next delivery would be VERY different. The birth of Carly, was traumatizing on so many levels. That I was only 21 and relatively immature and inexperienced probably didn’t help. I had wanted her very much and did everything to prepare, but like most of the cliches you hear about becoming a mother for the first time – nothing could have prepared me, especially for the frightening, dangerous, surgical birth.
Until my first daughter Carly was born by an ER-style emergency c-section, I had never been to the hospital except for the couple of times with minor injuries as a small child. The experience was so extraordinarily shocking to my system that it catapulted me into a determination that my next delivery would be VERY different. The birth of Carly, was traumatizing on so many levels. That I was only 21 and relatively immature and inexperienced probably didn’t help. I had wanted her very much and did everything to prepare, but like most of the cliches you hear about becoming a mother for the first time – nothing could have prepared me, especially for the frightening, dangerous, surgical birth.
After going through a rough post-partum depression, my reaction was to get pregnant again pretty quickly and immerse myself in research so that I could be more empowered the next time. I had been shocked into a state of alertness about my body and had a strong intuitive knowledge my next baby and I didn’t need to go through this same situation again.
I had done my homework and knew that what happened with Carly and I was unusual and not likely to repeat itself. I also learned everything I could about VBACs (Vaginal Birth After Cesereans). If my doctor had done a good job of patching me back together, and I believe that she had, my uterus and I stood a good chance of having the strength to give birth naturally.
Of course, this was 1985 and most OB/GYNs were not interested in risk-taking and were still not used to women and expectant parents empowering themselves to make these kinds of decisions. It was SOP (standard operating procedure – literally!) and understood that once you had a cesarean, you would ‘schedule’ your next one.
After confirming my pregnancy when Carly was only 8 months old, I started to search for an able and willing doctor who would work with us on a VBAC. To add to our young dramatic lives, we had just moved from New Jersey to Massachusetts, so I did not have access to the wonderful doc who had saved Carly’s and probably my life, AND who being the relatively rare woman OB/GYN, was more in tune with the whole VBAC thing.
My husband and I ‘interviewed’ many doctors, most of whom were not used to being asked detailed questions about their cesarean rates and feelings about safe VBAC options. I had one doctor actually say, “If that baby so much as farts, I’ll take it by c-section.” Needless to say, he was not our choice.
We finally found a wonderful man, Dr. Haling, who was really a midwife in a man-suit. He ran a beautiful and busy birthing center in Pittsfield, Massachusetts, which was right next to the hospital (which was a 45-minute ride from our home). We knew that because of the dangers associated with VBACs we were not candidates for the birthing center, but we accepted that quite readily and were thrilled to find Dr. Haling who understood our concerns and wish to have the most natural birth possible.
I found a wonderful natural childbirth educator named Debbie Lipp, who instilled a rock-solid foundation of knowledge and belief that my body could do this naturally and if intervention was necessary, we would know we did everything we could. She would later become my mentor as I also became a natural childbirth educator and labor support coach working specifically with VBACs.
Carly had come a month early, but had threatened to come even earlier, so we really weren’t sure how this one would go. My mother came up a month before my due date and camped out relatively patiently as we waited. We had a couple of false alarms, so we were good and ready when labor started in earnest one week early. Unlike the first time, it was kind of text-book normal – the early stage progressing slowly, but steadily. It had started late at night and we went to the hospital in the wee hours. I diligently practiced all my breathing, relaxation and coping techniques as things progress, but after 12 hours, my cervix was stuck at about 6 cenimeters and we decided to break the water and see if that would precipitate some action. Oh BABY! That little tired cervix responded by taking me from 6 to 10 in about 3 contractions – short but INTENSE transition!
We prepared to meet our tiny new babe. We had only had an initial sonogram and had opted not to learn the sex (if it were knowable at that time) and chose not to do any additional tests that could’ve revealed the sex.
Now it was time to do the work I had never gotten to do with Carly. I had done all I could to prepare. So, I started the pushing stage with excitement, focus and determination. I was planning to take a squatting position, but I quickly became aware of severe back pain in between the pushes, which rendered me nearly paralyzed and almost breathless and definitely speechless with pain. My husband wouldn’t have been able to support me properly between, so we propped me up on the bed and got busy. Pushing was relief. But after an hour the whole thing was getting exhausting to say the least. We had an external fetal heart monitor on and the baby was holding up well and presumably was in no hurry to meet us.
The staff was amazing. My husband and I were left alone a good part of the time. My husband was brave and never left my side and was enormously encouraging, but it was one female nurse who really saved me. Somehow looking into her eyes and hearing her say, “you can do this,” I knew it was true. I can’t remember her name, but it was this more than almost anything that led me to want to help other women through these intense moments, when a loving husband or well-meaning male doctor cannot with any REAL certainty say with authority that they understand.
By hour 3 of pushing, the doctor suggested that we use forceps, but he emphasized that he was only using them to turn the bean a little to help out. It seems in breaking the water we caught the wee one before the head was turned in the correct position and it needed a little help turning in the birth canal (Most babies are born face down, but if they come down face up or Octiput Posterior, that back part of the head is much harder and can be difficult to get past the tail bone).
He made an incision I’m not sure I even felt (later I learned that it went all the way to my anus and off to one side – ouch!) and then he barely touched the baby with the forceps and I heard them crash to the floor and within seconds I was holding my sweet little baby girl – Jessie. It was 6:06pm March 20, 1986, which also happened to be my sister Lisa’s birthday. So we named her Jessie Leigh (Lisa just didn’t work after Jessie, so it was close!). She was gorgeous (as all babies are to their parents) albeit wet and squishy from her trip into this world, and she was perfectly healthy. I kept her in my arms while the doctor did the grim task of sutchering me back together – honestly, I’m not sure which was worse, the c-section post surgical pain or the extended ‘hockey stick’ episiotimy I sported after Jessie’s birth!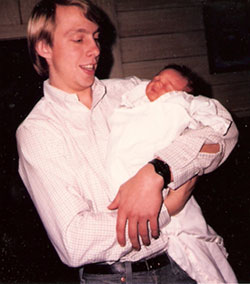
It was well worth it. An entirely different experience. Jessie had brought a lot of healing power with her and I developed a new or renewed confidence and trust in my body and the birthing process, which would help me later when I gave birth to yet another beautiful baby girl, Mary, completely naturally 7 years later, and would allow me to help other women as they faced similar birthing decisions.
That’s one of three of my stories. It was therapeutic to write it. We have fallen into a tradition of my telling each of the girls their birth stories on their birthdays. They all love hearing it, although it doesn’t really change from year to year! but, I don’t think I’ve ever written it out. A different process of storytelling that brings a slightly different perspective.
If anyone has any questions, I’m still fairly educated about these issues although it’s clearly been a few years since this birth event.
Photo credits: TOP – Not my belly! Photo used with permission from Relevant Times; BOTTOM – Proud daddy John Heissenbuttel with 1-day old Jessie Leigh Heissenbuttel, born March 20, 1986.
Great story. It is nice to hear of any type of VBAC today, with so many hospitals banning them. I had a VBAC with my second son in 2006. It was in the hospital, and even though there were things that I was not happy about, the overall experience was great-so much better than a C-section, and my recovery time was wonderful- I felt better after 3 weeks with the VBAC than I did after 12 weeks with the C-section.
Hopefully there will be a shift in the medical community and more and more doctors and hospitals will support VBAC’s.
What a great story to read. It’s so encouraging to the many other women out there who might be told today that they cannot have a vaginal delivery after C-section. I’m mostly impressed at the detail you recall after so many years – like it happened yesterday. That’s a testament to the indelible experience birth truly is!
My brother was born a VBAC (after I was c-section) and my mom had to strong arm her way into having it that way. I was so glad when I ended up having a vaginal birth, I was terrified of the thought of surgery! Thank you for sharing this incredible story. This is empowering and beautiful. I hope that all women who have c-section’s have a chance at a VBAC for their second, if they want it. Women deserve to feel empowered.